Preliminary discussion of national normal right ventricular function by real-time three-dimensional echocardiography.
Cai Jie, Wang Fang*, Zhang Ruisheng, Liu Hangyu,Wang Haiyan,Yin Dongmei, Li Jing, Zang Weier
Author Affiliations:Cardiovascular department of Beijing Hospital,Beijing,100730,China.
Abstract:Objective To validate the feasibility and accuracy of right ventricular(RV)volume and systolic function with single cardiac cycle real-time three-dimensional(3D) echocardiography. Method 3D images of RV and LV were obtained in 122 healthy adults by 3D matrix array transducer, the end systolic volume(ESV), end diastolic volume(EDV), stroke volume(SV) and ejection fraction(EF) were measured by RV analysis and left ventricle(LV) analysis software. To validate the reliability of measurement of right ventricle by real-time three-dimensional echocardiography,RV functional parameters were applied correlation analysis with multiple parameters (such as age,gender and BSA)respectively.And the correlation and difference between different modalities of left ventricle and right ventricle were compared. Result 3D-RVEF was 55.66±13.97%,3D-RVEDV was 68.24±40.19mL,3D-RVESV was 30.09±19.14mL,3D-RVSV was 38.30±26.10mL.RVSV and RVEF of normal men were more than those of normal women,but no statistical difference of them were found (RVSV:40.15±26.15mlvs36.11±25.60ml,RVEF:55.69±14.57%vs55.62±13.36%,P>0.05). RV related function parameters had no relevant correlation among different ages(P>0.05).body surface area (BSA) was weakly related to RVEDV,RVESV and RVSV(r=0.236,0.247,0.178,P <0.05).BSA didn’t relate to RVEF. 3D-RVSV, 3D-RVEDV weakly positive correlated with 3D-LVSV, 3D-LVEDV(r=0.215,0.201,P<0.05). 3D-RVEF, 3D-RVESV didn’t correlate to 3D-LVEF, 3D-LVESV.Conclusion the single cardiac cycle real-time three-dimensional echocardiography is a simple and feasible method for assessment of right ventricular function which in sampling mode and sampling information ,which can quantify right ventricular contractive function precisely.
Keyword:real-time echocardiography, right ventricle, contractive function
近年来,随着右心功能对先天性心脏病、心力衰竭、冠心病等一系列疾病预后判断的意义逐渐显现,其功能的评价日益被临床所重视[1-3]。但受右心室特殊的解剖结构及解剖位置所限,右室功能测定方法远不如左室成熟。实时三维超声心动图技术可在单心动周期内完成对心脏全容积图像的采集,且不基于心脏几何构型假设,可更真实地显示心脏的运动情况,在右心室功能评价方面存在独特优势。本研究旨在探讨单心动周期实时三维超声心动图测量正常人右心室容积及收缩功能的可行性及准确性。
资料与方法
一、对象
选取2013年9月至2014年6月来卫生部北京医院进行体检的健康志愿者及本院职工健康志愿者共122例,男66例,女56例,年龄(38.6±26.8)岁,体重指数(23.01±5.77)kg/m²,体表面积(1.77±0.35)m²。入选标准:窦性心律;正常范围心电图;体格检查及超声心动图检查无器质性心脏病者;图像质量佳者。排除标准:患有心肺疾病以及可能影响到心脏功能的疾病的患者,如慢性阻塞性肺疾病、肺动脉栓塞、心脏瓣膜病、先天性心脏病以及冠状动脉粥样硬化性心脏病、糖尿病、甲状腺疾病、肾脏疾病及恶性肿瘤患者等。
二、仪器与方法
采用西门子ACUSON SC2000超声诊断仪,4Z1c实时全容积探头,探头频率1~4 MHz,三维扇角90°×90°,深度12~16 cm,容积帧频>20帧/秒。系统自带左、右心室定量分析软件。
受检者取左侧卧位,嘱患者平静呼吸,常规接同步心电图,探头置于心尖,显示心尖四腔心切面。四腔心切面必须包括完整的左心室、右心室。按“4D”按钮进入容积成像系统,调节图像清楚显示右心室腔及心内膜边界(见图1),存储连续3个心动周期的全容积图像。选取拟分析的容积图,启动eSie LVA分析软件,自动计算出包括左心室射血分数(ejection fraction,EF) 、舒张末期容积(end-diastolic volume,EDV)、收缩末期容积(end-systolic volume,ESV)、每搏输出量(stroke olume,SV)在内的一系列参数,启动eSie RVA定量分析软件(见图2),包括标记三尖瓣、二尖瓣及左室心尖区中点,分别在四腔心冠状面、短轴横截面和右心室冠状切面手动描记收缩期及舒张期右心室内膜,软件自动追踪内膜运动,重构右室的结构同时得到反映右心室收缩功能的参数(见图3),包括右心室ESV、EDV、SV、EF。
三、统计学处理
采用SPSS19.0统计软件将右室、左室的心功能参数(ESV、EDV、SV、EF)进行统计学处理,结果均以均数±标准差(![]() )表示,右室SV、EF不同性别间比较采用独立样本t检验,右心室ESV、EDV、SV、EF与年龄和体表面积(body surface area,BSA)的相关性分析采用Pearson直线相关法,左室及右室功能参数间的比较采用配对t检验,两者的相关分析采用Pearson直线相关法,以P<0.05为差异存在统计学意义。
)表示,右室SV、EF不同性别间比较采用独立样本t检验,右心室ESV、EDV、SV、EF与年龄和体表面积(body surface area,BSA)的相关性分析采用Pearson直线相关法,左室及右室功能参数间的比较采用配对t检验,两者的相关分析采用Pearson直线相关法,以P<0.05为差异存在统计学意义。
结果
1、正常成人右室功能参数 应用右室分析软件测得三维右室EF为55.66±13.97%,三维右室EDV为68.24±40.19mL,三维右室ESV为30.09±19.14mL,三维右室SV为38.30±26.10mL(表1).
2、按性别分组后,男性受试者的右室EF和右室SV均大于女性受试者,差异无统计学意义(P=0.957,0.095)(表2)。
3、三维右室EF、EDV、ESV、SV均与受试者年龄无相关性(P=0.765,P=0.465,P=0.723,P=0.608)(表3)。
4、体表面积(BSA)与右室EDV、右室ESV及右室SV相关性分析r值0.178-0.247,呈弱相关性(表4),但与右室EF无相关性(P>0.05)。
表1 受试者临床特征 (共122人)
|
变量 |
数值 |
|
年龄(y) |
38.6±26.8 |
|
男性/女性 |
66/56 |
|
体重指数(kg/m²) |
23.01±5.77 |
|
体表面积(m²) |
1.77±0.35 |
|
3D右室EDV(mL) |
68.24±40.19 |
|
3D右室ESV(mL) |
30.09±19.14 |
|
3D右室SV(mL) |
38.30±26.10 |
|
3D右室EF(%) |
55.66±13.97 |
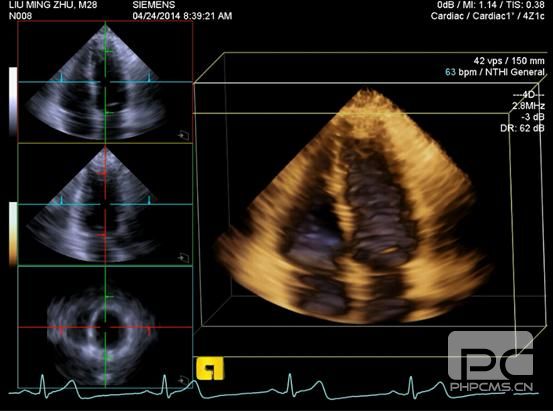
图1 实时三维超声心动图的心尖四腔心切面
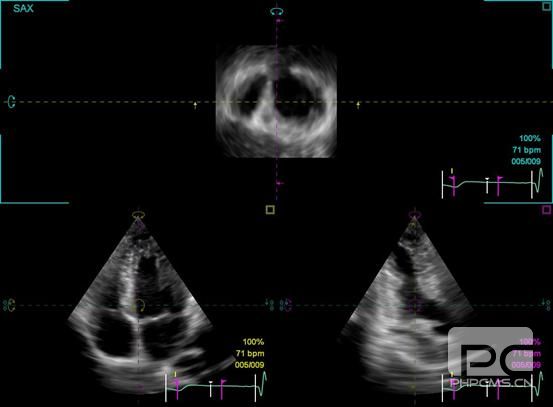
图2 右室分析标定三尖瓣、二尖瓣及左室心尖区中点示意图
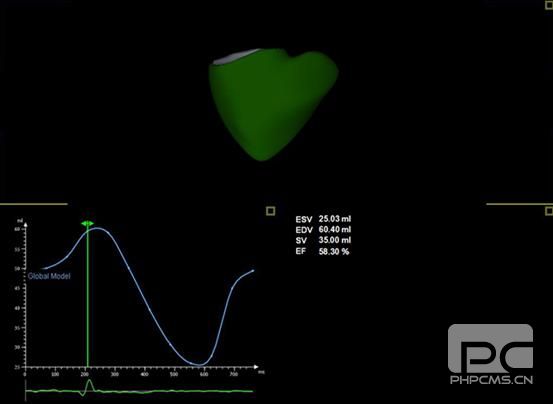
图3 正常人右室三维图像、容积、射血分数参数及右室容积变化曲线
表2 不同性别右室射血分数(EF)及每搏输出量(SV)独立样本t检验
|
受试者性别 |
EF(%) |
SV(mL) |
|
男性 |
55.69±14.57 |
40.15±
阅读数: 1953
|