1. Eric A. Rose, Annetine C. Gelijns, Alan J. Moskowitz, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345:1435-1443.
2. Andreas R. de Biasi, Keefe B. Manning, Arash Salemi. Science for surgeons: understanding pump thrombogenesis in continuous-flow left ventricular assist devices. J Thorac Cardiovasc Surg. 2015;149:667-73.
3. Emma J. Birks. Stopping LVAD bleeding. A piece of the puzzle. Circ Res. 2017 Sep 29;121(8):902-904.
4. Mandeep R. Mehra, Nir Uriel, Yoshifumi Naka, et al. A fully magnetically levitated left ventricular assist device-final report. N Engl J Med. 2019;380:1618-1627.
5. Jeffery J. Teuteberg, Joseph C. Cleveland, Jennifer Cowger, et al. The Society of Thoracic Surgeons Intermacs 2019 Annual Report: The Changing Landscape of Devices and Indications. Ann Thorac Surg. 2020;109:649-60.
6. Robert L. Kormos, Christiaan F.J. Antonides, Daniel J. Goldstein, et al. Updated definitions of adverse events for trials and registries of mechanical circulatory support: a consensus statement of the mechanical circulatory support academic research consortium. J Heart Lung Transplant. 2020 Aug;39(8):735-750.
7. Mandeep R. Mehra, Ivan Netuka, Nir Uriel, et al. Aspirin and hemocompatibility events with a left ventricular assist device in advanced heart failure. The ARIES-HM3 randomized clinical trial. JAMA. 2023;330(22):2171-2181.
8. Omar Saeed, Paolo C. Colombo, Mandeep R. Mehra, et al. Effect of aspirin dose on hemocompatibility-related outcomes with a magnetically levitated left ventricular assist device: an analysis from the MOMENTUM 3 study. J Heart Lung Transplant. 2020 June ; 39(6): 518–525. doi:10.1016/j.healun.2020.03.001.
9. Ivan Netuka, Peter Ivak, Zuzana Tucanova, et al. Evaluation of low-intensity and anti-coagulation with a fully magnetically levitated centrifugal-flow circulatory pump-the MAGENTUM 1 study. J Heart Lung Transplant. 2018;37:579-586.
10.Filippo Consolo, Giulia Sferrazza, Giulia Motolone, et al. Platelet activation is a preoperative risk factor for the development of thromboembolic complications in patients with continuous-flow left ventricular assist device. European Journal of Heart Failure (2018)20,792-800.
11.Alice Apostoli, Valentina Bianchi, Nina Bono, et al. Prothrombotic activity of cytokine-activated endothelial cells and shear-activated platelets in the setting of ventricular assist device support. J Heart Lung Transplant. 2019 June ; 38(6): 658–667. doi:10.1016/j.healun.2019.02.009.
12.Choon-Sik Jhun, Christopher Siedlecki, Lichong Xu, et al. Stress and exposure time on von Willebrand factor degradation. Artif Organs. 2019 Feb;43(2):199-206.
13.Nandan K. Mondal, Zengsheng Chen, Jaimin R. Trivedi, et al. Oxidative stress induced modulation of platelet integrin α2bβ3 expression and shedding may predict the risk of major bleeding in heart failure patients supported by continuous flow left ventricular assist device. Thromb Res. 2017 October ; 158: 140–148. doi:10.1016/j.thromres.2017.09.006.
14.Zachary B.K. Berk, Jiafeng Zhang, Zengsheng Cheng, et al. Evaluation of in vitro hemolysis and platelet activation of a newly developed MagLev LVAD and two clinically used LVADs with human blood. Artif Organs. 2019 September;43(9):870-879.
15.Ivan Netuka, Tomas Kvasnicka, Jan Kvasnicka, et al. Evaluation of von Willebrand factor with a fully magnetically levitated centrifugal continuous-flow left ventricular assist device in advanced heart failure. J Heart Lung Transplant. 2016;35:860-867.
16.Rashad Zayat, Ajay Moza, Oliver Grottke, et al. In vitro comparison of the hemocompatibility of two centrifugal left ventricular assist devices. J Thorac Cardiovasc Surg. 2019;157:591-9.
17.Omar Wever-Pinzon, Craig H. Selzman, Stavros G. Drakos, et al. Pulsatility and the risk of nonsurgical bleeding in patients supported with the continuous-flow left ventricular assist device HeartMate II. Circ Heart Fail. 2013 May;6(3):517-26.
18.Caren Taylor, Krystle Bittner, Nicholas Bartell, et al. Outcomes of gastrointestinal bleeding in patients with left ventricular assist devices: a tertiary care experience. Endoscopy International Open. 2020;08:E301-E309.
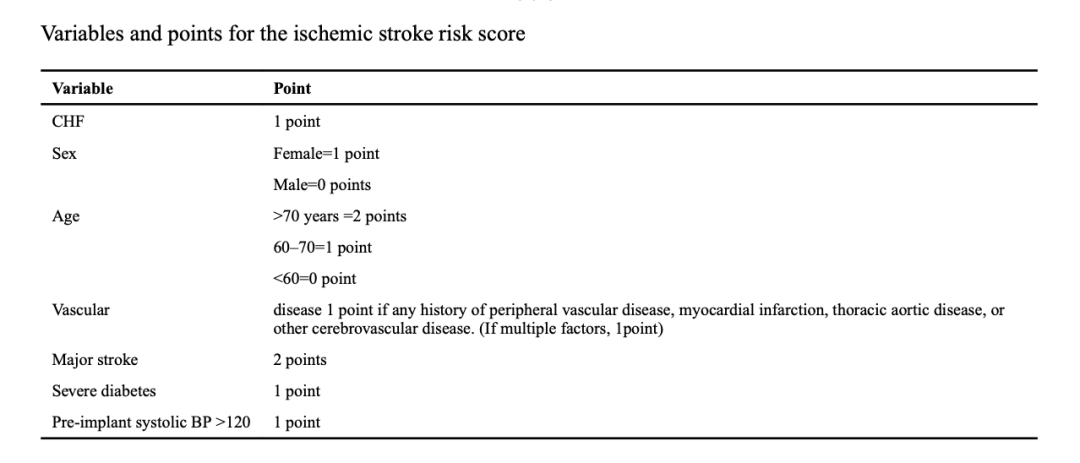
19.Deepak Acharya, Renzo Loyaga-Rendon, Charity J. Morgan, et al. INTERMACS analysis of stroke during support with continuous flow left ventricular assist devices: risk factors and outcomes. JACC Heart Failure. 2017 October;5(10):703-711.
20.Alberto Pinsino, Francesco Castagna, Amelia M. Zuver, et al. Prognostic impications of serial outpatient blood pressure measurements in patients with anaxial continuous-flow left ventricular assist device. J Heart Lung Transplant. 2019;38:396-405.
21.Teruhiko Imamura, Ann Nguyen, Gene Kim, et al. Optimal haemodynamics during left ventricular assist device support are associated with reduced haemocompatibility-related adverse events. Eur J heart Fail. 2019 May;21(5):655-662.
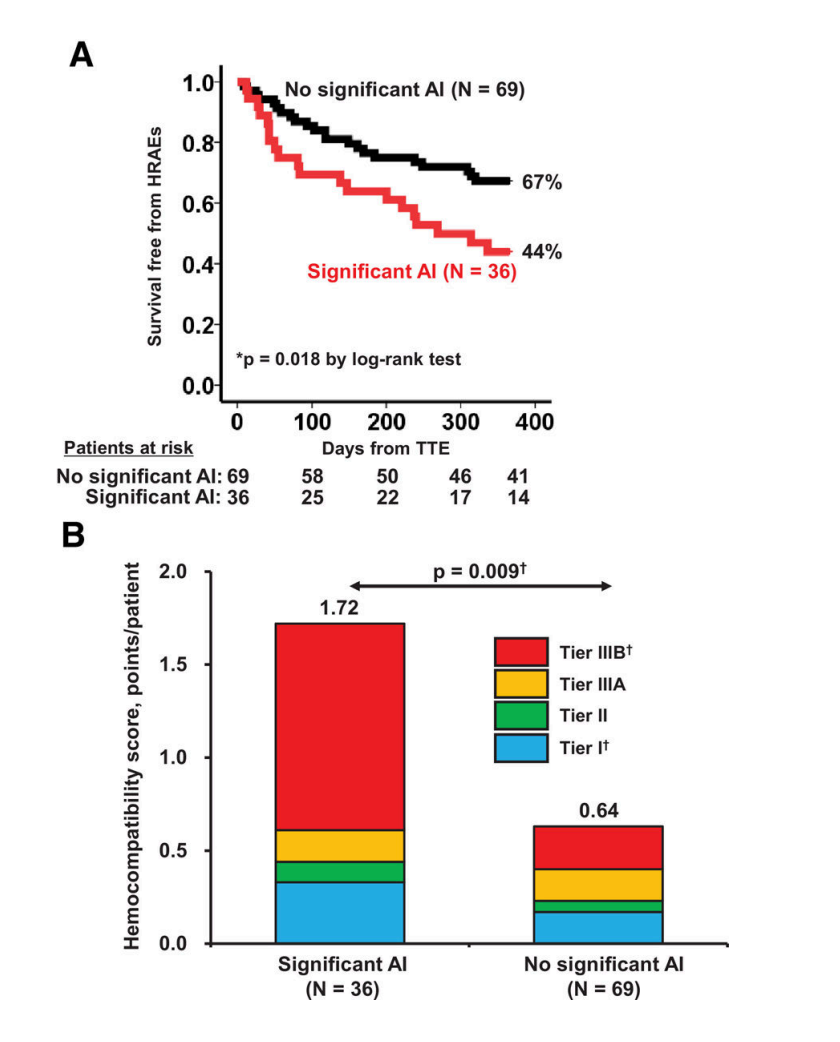
22.Teruhiko Imamura, Gene Kim, Daisuke Nitta, et al. Aortic insufficiency and hemocompatibility-related adverse events in patients with left ventricular assist devices. J Card Fail. 2019 October;25(10):787-794.
23.Saadia Sherazi, Peter Kouides, Charles Francis, et al. Prospective analysis of bleeding events in left ventricular assist device patients. Int J Artif Organs. 2018 May;41(5):269-276.
24.Jennifer A. Frontera, Randall Starling, Sung-Min Cho, Amy S. Nowacki, Ken Uchino, M. Shazam Hussain, Maria Mountis and Nader Moazami, Risk Factors, Mortality and Timing of Ischemic and Hemorrhagic Stroke with Left Ventricular Assist Devices, Journal of Heart and Lung Transplantation, http://dx.doi.org/10.1016/j.healun.2016.12.010.
25.A. Montalto, M. Comisso, A. Cammardella, et al. Early Aspirin nonresponders identification by routine use of aggregometry test in patients with left ventricle assist devices reduces the risk of pump thrombosis. Transplant Proc. 2019 Nov;51(9):2986-2990.